Gov. Tom Wolf toured the facility that hopes to provide more than 3,000 vaccinations by the end of April.
York health provider sets sites on COVID vaccines for underserved community
York, PA — Starting tomorrow, a new vaccine clinic will throw open its doors in York, targeting the underserved community.
“It’s one of the puzzle pieces. This is not a mass vaccination site but serves a very specific precision purpose,†said Jenny Englerth, President and CEO of Family First Health.
Because the number of people from these communities getting immunized is staggeringly low, Family First Health is kicking off March Madness. The goal is to turn the three-story York location into a vaccine clinic, serving 200 to 300 people, every Friday, that might have shied away from getting the medicine from an unfamiliar place.
“Family First is a great example of how federally qualified health centers and local providers can serve vulnerable populations,†said Governor Tom Wolf.
Gov. Tom Wolf praises York health center for efforts to vaccinate underserved groups
YORK, Pa. —
Gov. Tom Wolf is praising a community health center in York for its commitment to vaccinating underserved groups.
Wolf visited Family First Health on South George Street on Thursday to thank staff and tour the COVID-19 vaccination area.
The governor said federally qualified health centers, including Family First Health, have played a big part in ensuring that vaccines get to the vulnerable populations who need them through direct outreach to patients.
“I really appreciate coming to places like this because we can all learn a lot from the good things that are happening here,†Wolf said.
The health center is gearing up for a boost in its vaccination efforts. Starting this week, it will offer all-day Friday vaccination clinics.
“We’re always looking for ways to do a better job,†Wolf said.
Family First Health has vaccinated about 1,000 people since late December. With the Friday clinics, the goal is to vaccinate 3,000 people between now and the end of April.
Family First Health, local doctors hold virtual COVID-19 vaccine Q&A
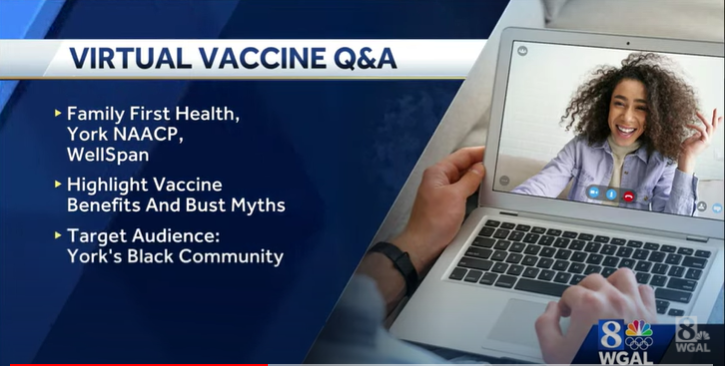
YORK, Pa. — Family First Health is organizing a virtual Q&A with local doctors about the COVID-19 vaccine.
Vaccine Q&A details
- The forum will be held Tuesday evening from 6:30 p.m. to 7:30 p.m.
- You can watch and ask questions through the Family First Health’s Facebook page or YouTube channel.
COVID-19, one year later: Coronavirus exposed racial inequalities in Pa. What comes next?
About this series: Over the next several weeks, reporters with USA Today’s Pennsylvania network will take a look back at the impact COVID-19 has had on the commonwealth over the past year, and what the future holds.
Neighborhoods across the state — some lined with million-dollar homes, others by more modest dwellings — struggled to survive this year as the coronavirus pandemic uprooted the lives of Pennsylvanians everywhere. But while the unprecedented catastrophe was shared by millions adjusting to their “new normal,” the suffering was not equally spread.
For low-income Pennsylvanians like Elena, a mother of two without reliable income to pay the bills, surviving the pandemic was made harder by financial and structural imbalances that almost ensure the most marginalized residents bear the heaviest burdens of a public health crisis.
Elena, who requested her last name not be used, is part of both the Latino and immigrant communities in Pennsylvania.
In the last year, she and her husband lost their jobs to the coronavirus pandemic. She was a dishwasher, and he was cook at a pizza restaurant. By the end of March, her whole household had contracted the virus.
“Myself, my husband and my two children suddenly fell ill, and we didn’t know where to go and I didn’t know what to do to save their lives,” Elena, 49, said, her voice quivering as she shared the memories. “The only thing that I could do was cry and ask my god not to take away my life or my family.”
In her desperation to keep her children healthy, she went without eating a meal for days, giving any food they came by to her kids. They had made it through the pandemic — “barely,” she said — surprised but grateful her family recovered from the virus and managed to keep a roof over their heads.
“Life is very sad when one has children and does not have any food — or even a single penny to buy any food,” Elena said. “I don’t even want to remember those times. I remember my kids crying, asking me to do something and I couldn’t do anything. I couldn’t even go to the hospital because we didn’t have health insurance.”
‘Stark and noticeable’ differences as the virus spread through communities
Tonya Larry, 52, noticed something spreading in her Facebook timeline in the first months after the novel coronavirus’ arrival was announced in Pennsylvania.
She was posting about the illnesses and deaths of her friends, family, and acquaintances to COVID-19; her Black Facebook friends were doing the same.
Her white friends were not.
It was the painfully personal, real-time, live-update truth of the statistics that would become well-known: that the Black Pennsylvanians making up just 12% of the state’s population were, in those early days, making up more than 30% of COVID-19 deaths.
“I would literally have friends — white friends — that would say, ‘I don’t know anybody who’s gotten it or died.’ … To me, it was very stark and noticeable,” said Larry, of York, who contracted the virus in July and recovered.
That changed over time as the illness spread across communities, she said. Still, few of her white friends reported knowing 5 or 10 people who had died, as her Black friends knew. Like she knew.
Sometimes called the great equalizer, the novel coronavirus has been anything but.
As the pandemic has continued, low income Pennsylvanians of color bore some of the heaviest weight of the virus, though it can be hard to see that clearly in the data provided by the state department of health.
At face value, the 81,180 Black people who tested positive for COVID-19 is less than the 487,131 white people who tested positive in Pennsylvania. The same is true for the 2,829 Black people who died from the coronavirus and 19,497 white people who died.
But when you consider that 82% of the state is white, and 12% is Black and, it’s easier to see how the minority community has been disproportionately impacted.
Several experts who spoke with the USA Today Network, such as Dr. Georges Benjamin, executive director of the American Public Health Association, attributed the initial racial gap to the long-term discrimination and structural racism rooted in our soil since long before COVID-19 touched down.
What’s harder to say is what these effects will mean after COVID-19.
COVID-19, one year later: Pennsylvania hospitals deal with financial, emotional toll
The state has made significant strides during the pandemic, but problems developed over four centuries can’t be dismantled by a single task force over a series of months, Benjamin said.
“I’m glad the issue of health inequities and disparities is being elevated, but it is sad that we are seeing this disparity play out time after time,” he said. “It will happen with the next pandemic that comes along if we don’t pull ourselves together as a society and commit to addressing it.”
Where it hurts Black and brown communities
Racial health disparities were known long before COVID-19 was a blip on a world news briefing in the U.S., said Dr. Matt Howie, a primary care physician who serves as a health strategist for WellSpan Health Network and is helping coordinate their COVID vaccine distribution plan.
Howie, who is also medical director of the York City Bureau of Health, has been dedicated to building trust in communities typically underserved by the state’s health care system.
“We understand a little bit more now about what some of the underlying issues are, but there are intractable issues … some of them are things like education and income and other things which are bigger societal problems,” he said.
Some of the preexisting conditions most likely to result in severe illness from COVID-19 are the same ones disproportionately affecting Black people in the U.S. These include diabetes, obesity, and heart conditions.
But, as has been said before, the true preexisting condition is racism, Benjamin said.
“There is nothing that says someone who is born with a particular amount of melanin in their skin, therefore, should have a higher rate of these health conditions,” Benjamin said. “It is absolutely the conditions into which they are born and how they are treated in society that cause these disparities to exist.”
It starts with the founding of the country, Howie said, and bleeds through generation after generation, affecting different aspects of life — from where people live, to the jobs they have, to the educational opportunity they get to the foods they eat.
It comes down to one other, related idea, by the telling of Sal Galdamez, of York.
Galdamez, 48, moved to the United States at the age of 9. A native of El Salvador, he was an orphan relocated to South Central Pennsylvania. Galdamez finally felt at home when he moved to York about nine years ago.
“The white folks have more money than we have and there’s more poverty in the Black and brown communities,” he said.
The practice, which used race to deem neighborhoods “hazardous,” meant mortgage loans weren’t given in Black neighborhoods. Maps that used red to line the areas were drawn up in the 1930s and the practice was outlawed in the 1960s, though an investigation by Reveal from The Center for Investigative Reporting found echoes in modern-day mortgage lending in the commonwealth.
White families given nice loans in the suburbs got to see their additional financial leg-up benefit the next generation, Galdamez said.
“You ended up having very concentrated poverty — strategically so — in communities of color,” he said. “And so when you do not have access to capital and money to have secure housing, that has spiraling consequences for not just you but generations that come after you.”
When a community has more people with less income, it means a smaller tax base for good schools, Howie said. People forced to work multiple jobs to make a living may not have the time or finances or access to fitness centers for healthy exercise. Their neighborhoods, also, may not be safe for outdoor workouts if people do have time. The stress of the situation can also lead to health concerns.
Then there’s access to healthy food.
“Sometimes you don’t have the money to go to the grocery store,” said Anu Banks, who stopped by Union Lutheran Church in York City on Wednesday to hand out groceries from the food pantry.
Banks said those become meals for several days for many community members.
Communities that have been underinvested often have fewer grocery stores, Banks said. Grocery stores also might be hard to get to, he said, making it less likely that people are able to get to good grocery stores with the quality ingredients to keep them healthy.
More: These Pa. residents never thought they’d be here – in line at a food bank in a pandemic
“Some people don’t have the access, because they don’t have the transportation,” Amanda Cree said when she recounted the struggles her family has endured the past year because of the pandemic.
Within the last year, the Dauphin County mother of two has lost both her job and her roommate. She was working as a delivery driver for Uber and DoorDash before leaving her job to stay at home with her immune-compromised twin sons.
Cree relies on food pantries to help supplement her grocery bill, she said. It helps her pay other bills while she raises her children, and, on top of that, the quality is often good, she said.
That isn’t the case at grocery stores near her home, where food appears to be old and backdated, she said.
Lack of transportation also means less ability to get to a health care facility, less ability to get to one that accepts a specific health insurance provider, and less ability to get diagnosed and treated, said Jenny Englerth, President & CEO of Family First Health, a not-for-profit health care system dedicated to providing quality and cost-effective care in urban and rural communities throughout south central Pennsylvania.
And that’s if someone has health insurance to begin with.
Because of the obstacles, members of communities of color may only go to the hospital when their health conditions get really bad, Englerth said.
“And usually, by that time, they’ve probably got something that’s not as easy to reverse,” she said.
Where it got worse for minority groups
The stage was already set and slanted against the Black and brown population. Then March 2020 arrived, along with the announcement of the first known COVID-19 case in Pennsylvania.
The problem wasn’t just the overlapping preexisting conditions between communities of color and COVID-19’s worst cases.
Lack of testing, lack of information, and nonsensitive linguistics in messaging all worsened the situation for these communities, said Brian Lentes, director for the Office of Operational Excellence at the Pennsylvania Department of Health.
The impact of health disparities is exponential.
“The disparities compound each other, and COVID-19 compounded the issue,” he said.
Take, for example, that on average about 2.2 million Pennsylvania residents face food insecurity annually. Yet, during the first three months of the commonwealth’s COVID-19 response, food banks served more than 5.5 million people, according to Feeding Pennsylvania.
“Some people that were hanging on, sort of on the edge, COVID just kicked them off the ledge,” Englerth said.
Even the suggested methods of combating COVID-19 — staying home, social distancing, using separate bathrooms when ill — didn’t recognize the disadvantage for the communities of color in fighting COVID-19, she said.
Research has found that higher-paid employees are more likely to have the option to work from home, and that Black and Hispanic employees are less likely to be able to work remotely. In Pennsylvania and across the country, front-line employees like janitors, grocery clerks and transit workers are more likely to be women and people of color, an analysis of U.S. Census Bureau data revealed.
That’s forced low-income workers and people of color to risk their health at work, exposing them to the virus while others earn a paycheck from home. Some had to ride public transportation, increasing exposure.
Allegheny County bus driver Patrick Hazlett had to work on public transportation. He died of COVID-19 after raising alarms to his family about how some passengers would cough on drivers who told them they needed to wear a mask on the bus, according to media reports.
Some people might not have had a paid leave option, Englerth said. Some people may not have been able to get to testing. And those who tested positive were told to stay home and use a separate bathroom than other family members.
“If you are more likely to live in poverty, how can we expect you to use your own separate wing of your home when you’re just trying to make it and you’re maybe living on your couch, or maybe you’re in multigenerational housing, which is not always necessarily affiliated with poverty, don’t get me wrong there,” Englerth said.
“But it just makes every single step more challenging, and that’s why we’re seeing the disparities with COVID-19. Just like many other diseases.”
How is Pennsylvania fighting back?
The COVID-19 Response Task Force, led by Lt. Governor John Fetterman, was formed in mid-April to address growing concerns about how the coronavirus was disproportionately affecting minorities and adding to existing health disparities.
“It’s unconscionable for Black, Hispanic, and Asian-Pacific Pennsylvanians to be hit harder by this pandemic, which has highlighted the systemwide inequity that already existed in these communities,” Fetterman said when the task force was created.
The state started working to improve its data collection to get a better understanding of how the virus was affecting various groups of people.
But almost a year into the pandemic, coronavirus data on race and ethnicity was still lagging on the state health department’s website.
The state made progress on collecting that information from medical providers, but there’s still about 364,000 cases with no race or ethnic data, according to the dashboard.
Pennsylvania was a leader in terms of doing the right thing, Gov. Tom Wolf said. But there’s still more to do.
Benjamin’s mind is on Wolf’s “lofty” but “achievable” goal to avoid disparities in vaccine access, he said, applauding the strategy. Wolf also wants to assure vaccination access to disproportionately harmed groups.
To date, over 2.1 million Pennsylvanian residents have been vaccinated, but only about 1.2% of those people are African American and .5% are Hispanic, according to the DOH’s vaccine dashboard.
The state is addressing the vaccine concerns with an equity-focused strategy and extra doses outside the main strategy, acting health secretary Alison Beam said during a health committee hearing in February.
Beam also addressed concerns for vaccination data collection, which she said the state is improving the entry process for and will release soon.
Still, there remains the longer term, harder-to-tackle tasks.
Long-term consequences after COVID-19
The pandemic’s effect may ripple through minority communities in the years to come.
“That is something that keeps me up at night,” Larry said.
She is concerned about the long-term health consequences believed to be associated with COVID-19. She’s concerned for the mental health of the Black children who have been orphaned or now have a parent with those long-term health consequences. She’s concerned the economic impacts will hurt communities that were already struggling.
“Down through time and through generations, we are going to feel the loss — such an abrupt loss — of so many people of consequence, because these are people of accomplishment,” Larry said.
Benjamin has hope, however. He couldn’t do this work otherwise.
COVID-19 may not have uncovered health disparities, but it made them more widely known, he said — the public can no longer claim ignorance of the issue.
“We’re well past the ‘Aha moment’ that health disparities exist,” Benjamin said. “Now, it’s time for plans that are community-based, not top-down, and at every level of governance and society.”
Anika Jackson Featured on WURD Radio

In case you missed the February 23rd episode of Reality Check with Charles Ellison on WURD Radio, Anika Jackson, our Director of New Initiatives was featured to discuss COVID-19, Trust, and Vaccines.
Reality Check features thought leadership, analysis, and data on the politics, policies, and people impacting our communities in Philadelphia and on the national and international front.
Reality Check with Charles Ellison airs every Monday through Thursday (when City Council is not in session) from 10am-1pm . Each day features important thought leadership, analysis and data on the politics, policies and people impacting our communities here and abroad. Veteran political strategist and Philly native, Ellison presents the issues rippling through the nation’s capitals, state houses, city halls and neighborhoods. If you need a #RealityCheck, tune in! Join the social media discussion @ellisonreport.
Anika Jackson Featured on WITF’s Toward Racial Justice

Anika Jackson, the Director of New Initiatives at Family First Health was a panelist on the February 18th broadcast of WITF’s Toward Racial Justice.
Toward Racial Justice: COVID-19, Trust and Vaccines explores some of the racial disparities within the COVID-19 pandemic. We also look at the hesitancy regarding vaccines. (Broadcast live on Feb. 18)
Panelists:
Rev. Dr. Brenda Alton
Dr. Marilyn Corder
Dr. Eugene Curley
Anika Jackson
Dr. Mary E. Kelleher
Dr. Ivan Walks
FFH Physician Joins Caring Together Care Team
York, PA – December 1, 2020: Oluwatomi Uwazota, MD, primary care physician at Family First Health, recently joined our Caring Together team that provides comprehensive medical services to patients living with HIV. She has also recently completed her MS in Public Health from the Johns Hopkins Bloomberg School of Public Health.
Dr. Uwazota joined Family First Health in 2019. In her relatively short time at Family First Health, she has found that the knowledge gained from her patients she has learned that their overall health is truly a function of where they live, work, learn, and play, as well as their social network and other support structures. She frequently engages both clinical and non-clinical team members who can help address barriers that our patients face. During patient visits, she actively finds ways to engage family members and the patients together because of her strong belief that patients’ families play an invaluable role in helping the patient succeed. Using the tools afforded her by her public health training allows her to troubleshoot challenges she encounters as a medical provider as well as issues that she faces within her team, looking for ways to continue to serve our patients better.
On her recent inclusion on the Caring Together team, Dr. Uwazota remarked: “This is very exciting for me because I get to work within an incredible team of people who are already applying the ecological construct to influence behavior and achieve better health for our patients.â€
Through Family First Health’s Caring Together program, we offer a seamless system of coordinated, high-quality care for people who are HIV positive, so they can access the services they need. Family First Health also offers free, confidential HIV testing and counseling for individuals age 13 and older at our George Street Center. Interested individuals can call 717-846-6776 for more information.
About Family First Health
Founded in 1970, York Health Corporation, now Family First Health, is a nonprofit Federally Qualified Health Center dedicated to providing accessible, high-quality health care at seven convenient locations in Adams, Lancaster, Lebanon, and York counties. Family First Health strives to improve the health of all members of the communities we serve through primary medical and dental care and a wide range of community health programs. Our uniquely qualified team of health care professionals creates an environment that is patient-centered, helping patients to live happier, healthier lives.
For more information, visit www.FamilyFirstHealth.org. Se habla Español.
New Partnership Expands Access to Care for Pennsylvania Families
United Health Foundation and Family First Health, a federally qualified health center, are joining forces to improve access to health care for children and their families across Pennsylvania while widening the reach to serve vulnerable populations.
United Health Foundation’s three-year, $2 million grant to Family First Health will enhance services at Family First Health’s York, Pennsylvania, location, a school-based health center housed at Hannah Penn K-8 school, home to a significantly underserved population. The grant will help the school’s health center connect students, families and school staff to expanded primary care services as well as offer new behavioral health and wellness resources to the school’s students.
The program will also deploy “Health Connectors,†health care professionals who will provide in-home support to families, such as helping individuals manage chronic conditions. Health Connectors will also connect families to the providers at the Hannah Penn Center and help those eligible enroll in health insurance.”Family First Health is connecting students to primary care, as well as additional services that help them to be healthy and ready to learn.”
“Family First Health is connecting students to primary care, as well as additional services that help them to be healthy and ready to learn. This is incredibly needed and important during these historic times,†said Pennsylvania Governor Tom Wolf. “On behalf of York and the entire state, I want to thank the United Health Foundation for its support of this innovative health model and its commitment to children and families at their most foundational times.â€
Hannah Penn K-8’s school district ranks among the highest in the state for acute poverty. The socioeconomic challenges in the district translate into a high transiency rate, with a roughly 23% student turnover during the 2018 school year.
“The United Health Foundation is committed to improving and expanding access to health care in Pennsylvania,†said Marynell Benson, a regional president of Optum Complex Care Management. “Together with Family First Health, this partnership will support underserved families with expanded primary care services as well as behavioral health and wellness resources.â€
The health center at Hannah Penn K-8 School.
While the grant partnership was initiated prior to the COVID-19 outbreak, the onset of the pandemic makes the collaboration even more timely. Overall, UnitedHealth Group has contributed more than $100 million to fight COVID-19, support impacted communities and address emerging health care issues related to the pandemic.
“Family First Health is committed to providing primary medical and dental care, integrated behavioral health and substance misuse treatment services to Pennsylvania residents regardless of their ability to pay,†said Family First Health CEO Jenny Englerth. “This generous grant from the United Health Foundation is especially critical during this unprecedented time because it will allow Family First Health to help underserved populations obtain the care they might not have otherwise received during school closure and stay-at-home orders.â€
Find the full article: https://www.unitedhealthgroup.com/newsroom/posts/2020-10-22-united-health-foundation-family-first-health-expand-access-423628.html